AI-Driven Medical Coding
📌Automated, Accurate, and Efficient
📌Reduce errors, streamline claims
📌Accelerate reimbursements with AI-powered coding.

Try Our Interactive ROI Calculator and see how you can realise tangible benefits
Current monthly patient volume
Total number of patients seen at your facility each month. This helps estimate how often medical coding is required.
Average number of medical claims processed per month
How many claims your team handles monthly for insurance billing and reimbursements. Affects total workload and savings potential.
Average cost per denied claim
Estimated financial loss for every insurance claim that’s rejected due to coding errors or missing data.
Time spent on manual coding per claim
Average number of minutes your medical coding staff spends reviewing and entering codes manually for each patient case.
Average hourly wage of medical coders
Hourly salary or contract rate you pay per medical coder. Used to calculate labor savings with automation.
Number of medical coders in the team
Total number of medical coders currently working in your organization. Helps determine potential productivity improvements.
Your ROI results explained
Help healthcare organizations calculate the cost savings and efficiency gains from reduced medical coding errors, streamlined claims processing, and improved reimbursements.
AI Medical Coding
ROI Calculator
Coder information
ROI Results
Nexpert’s AI-powered coding assistant simplifies medical coding, ensuring compliance with regulatory standards:
ICD-10
CPT
CCAM
Riziv/INAMI
Medical Billing
Faster Medical Billing – Cut manual work by 40%
Compliance
Higher compliance – Align with global and regional coding standards.
Coding Validation
Real-Time Coding Validation – Reduce financial losses from incorrect submissions.
No posts or pages added.
Want a personalized demo?
Schedule demo with Nexpert team to find out more about how the solutions can best fit your needs
GET DEMO
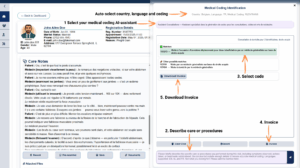
Advanced Prompt Engineering
Medical Coding
Nexpert leverages AI-driven prompt engineering to enhance accuracy in medical coding.
Example: A doctor enters patient symptoms → AI generates suggested ICD-10, CPT, CCAM, or Riziv/INAMI codes automatically.
Nexpert’s engineered prompts structure the AI request, ensuring more precise and relevant coding recommendations.
GDPR-Compliant Data Processing with AI
Compliance
AI anonymizes patient-sensitive information before processing coding requests.
Only essential clinical details are sent to AI for analysis.
Ensures full compliance with GDPR, HIPAA, and local healthcare regulations.

Automated Code Validation & Compliance Checks
Validation and Claims
AI cross-references coding suggestions with regulatory databases.
Prevents coding errors that lead to insurance rejections or claim denials.
Ensures regional compliance for coding frameworks across Europe, the U.S., and global markets.

Integrated AI Learning from Previous Coding Patterns
Accuracy
AI learns from past user selections and corrections, continuously improving coding accuracy.
The system adapts to individual clinician preferences, making suggestions more personalized over time.

(Future expansion)
Speech-to-Code Automation
Direct integration with speech-to-text tools.
Clinicians can dictate patient encounters, and AI automatically generates medical codes based on voice input..
Reduces documentation burden and accelerates medical billing workflows.

Multi-Specialty Adaptation for Different Medical Fields
Code adjustment
AI dynamically adjusts coding for various specialties, including:
✔ Primary Care – Chronic disease management, routine check-ups
✔ Surgery – Procedure-based coding for CPT/ICD-10
✔ Mental Health – Behavioral health-specific billing codes
✔ Radiology & Imaging – AI-assisted interpretation of scans
✔ Emergency Medicine – Automated triage-based coding

FHIR-Based Integration for Seamless Medical Billing
Billing
Syncs AI-generated medical codes directly with EHR and billing systems via FHIR API.
Eliminates the need for manual code entry.
Ensures real-time billing validation before claim submission.

How it works:
- The system analyzes consultation notes
- AI suggests appropriate medical codes.
- The user validates or adjusts the code before submission.
